
Summary
Sexually transmitted diseases, or STDs, are infections you can get from having some form of sex. Some STDs are infections of the genitals (penis and vagina), mouth and throat or backside (anus), and some involve infections in the blood and body more generally.
STDs are common, but manageable. They can cause a lot of distress and panic; however once you know more about them, you can plan ahead to cut down your risk and manage your exposure to STD to get rid of the distress and get on with your life.
Anybody who is having sex outside of a one-partner long term relationship should consider STD testing. What STD you should be tested? It depends on what kind of sex you have and with how many partners. What you need to be tested for? This is based on your individual risk.
This guide talks about common STDs, how they are caught, what symptoms they have, how they are shared and what to do about them.
We will also talk more about how some STDs are caught, whether it means you have been cheated on and how to know that you have gotten rid of an STD.
Introducing Sexually Transmitted Diseases
Patients from all walks of life seek STD screening. For some, this is an embarrassing experience but it need not be. STDs are part of life and treatment is available. Doctors are trained to handle any issue professionally with context and compassion ,and a good one will be helpful and non-judgemental. It is also a good opportunity to discuss other issues such as lifestyle, exercise, vaccines, cholesterol etc., which many people forget to see their doctor about.

How do sexually transmitted diseases spread?
STDs spread by the close contact with the skin, fluids or blood of another person. Oral, vaginal and anal intercourse all involve close contact with potential reservoirs of disease. Where I come from, we regard this as ‘sex’.
In order to catch an STD, there is contact of a non-infected person with an infected person so that the virus or bacteria can transfer. One thing to note is that this does include the throat where chlamydia and gonorrhoea can lie in waiting to be transferred.
As such, oral sex still requires testing for STDs as it is a similar point of contact for all diseases able to affect other sexual organs.
Where can you get STDs?
Sexual infections can be found typically in the three main (sexual) areas: the throat, anus (the backside) or genitals.
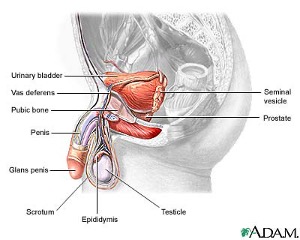
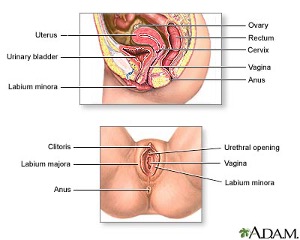
Genitals here refers to the all the bits of the sexual organs including the epididymis, testicles and perhaps prostate in men and the vagina, cervix, uterus, fallopian tubes and associated pelvic cavity in women and the nearby lymph glands.
Some infections will be caught from these areas and transfer to the blood stream such as syphilis, hepatitis B and C and HIV; these are called ‘blood borne’ infections. They are more rare than the infections you get near the genitals and are a higher risk in certain groups of people.

What kinds of STDs are there?
Infections of the mouth, anus and urethra:
Chlamydia, Gonorrhoea, Mycoplasma and Ureaplasma are all bacterial organisms that are known to be sexually transmitted. They tend to infect the genitals via the ‘urethra’, the tube that urine comes through.. As such, they were traditionally referred to as the ‘urethritis’ organisms.
These organisms, however, do not just infect the urethra. These bacteria can infect the throat, anus, cervix, fallopian tubes, prostate and testicle itself and present in multiple different ways ranging from painful urination, discharge, swollen testicle, painful defecation, bleeding after sex, pain after sex, anal discharge and non specific abdominal pain, throat pain or fever.
Sometimes these infections give you symptoms but many people do not have obvious symptoms at all; from this, the bacteria can hang around for years slowly causing scarring or will wait ready to infect a partner later on.
Other STDs are infections that enter the body and can spread more broadly. These include the blood borne viruses such as Hepatitis B, C and HIV as well as syphilis. We will discuss them later.
What parts of my body should I test for STDs?
Based on your sexual activity, you should be tested for STDs in all areas involved in the sexual exposure and be treated and then tested again in all those areas to make sure that the infection is cured.
That means if you engage in oral or anal sex too, you will need to test these areas with a swab. A swab looking for chlamydia in the urethra or vagina will not be able to identify chlamydia in the throat or gonorrhoea in the anus.
Furthermore, none of these diseases leaves behind immunity and so it is possible to catch it again right after treatment.
In a phrase; test for ALL possible STDs in ALL possible areas after ALL exposures.
Who should be tested for STDs?
Anybody who is having sex outside of an entirely monogamous relationship should have an STD test. This is because it is possible for anybody to give you an STD.
If you are in a new relationship, partners will often get tested in case themselves or their partner bring ‘something to the table’. This might be a limited test looking for the most common or likely STDs or something more comprehensive based on a person’s sexual history.
Does having an STD mean my partner has cheated on me?
Not really. There is no benefit in ‘pointing the finger’ if your partner has an STD. It is possible they had it from years back during a previous relationship and may very well have had no symptoms and just never knew. This could occur to anybody; so just get tested and treated and move on with life. STDs do not always suggest cheating.
Do gay men have a different recommendation for STD testing?
Gay men have a unique recommendation for STD screening involving rectal, throat and urethral swabs for chlamydia, gonorrhoea and syphilis/HIV/Hep C blood tests every 3 months. This is a good chance to discuss PrEP.
This is because different STDs occur in this population.
Other than this, STDs testing is determined on the basis of risk and sites involved. If somebody has many partners or engages with sex workers, it might be better to test more widely for STDs.

Who is a higher risk for an STD and what should be routinely tested?
High risk describes a cohort of people who, based on sexual behaviour, are more likely to be exposed to an STD. This cohort may include:
- Men who have sex with men
- Sex workers
- IV drug users
- Unknown partner status
- Many partners
Whilst most encounters are unlikely to warrant a full STD panel however the discussion should take place with your doctor.
For high risk exposures with no symptoms, the following tests are recommended:
- Urine chlamydia and gonorrhoea test
- Throat/Anus swabs for chlamydia and gonorrhoea (if applicable based on sexual practices)
- Syphilis/HIV/Hep C Blood test
High risk should be tested every few months and consider a medication that helps prevent HIV called PrEP. We will discuss that medication later.
For high risk exposures with symptoms, the following tests are recommended:
- Urine/Urethral swab testing for chlamydia, mycoplasma, ureaplasma and gonorrhoea test
- Throat/Anus swabs testing for chlamydia and gonorrhoea (if applicable based on sexual practices)
- Syphilis/HIV/Hep C Blood test
- Urine microscopy and culture (testing if anything grows from the urine)
- High Vaginal Swab microscopy and culture if applicable.
At the most basic level, all people not with one partner all the time should have a urine test for Chlamydia and gonorrhoea once per year.
What is it like to get an STD check with your doctor?
During an STD consultation it is often not necessary to dive into every detail of your sex life and it is usually not necessary to take clothes off for a physical examination.
Often, a description of the problem is enough to proceed with tests and treatment and results can be given by email or by phone and leave treatment for pickup.
Will I be embarrassed?
Sex is a part of life and nobody wants an STD or ‘deserves’ one.
A caring doctor who is realistic about sex in the 21st century is essential to ensure that these little issues are sorted out , and that you can be safe, get on with your life and put your mind at ease.
This guide aims to make it easier to seek help regarding sexual medicine.
No matter who you are, get tested and get treated; the embarrassment might last 30 seconds but the relief will last much longer!
Explanation of Jargons
Urethra: The tube that you urinate from, comes from the bladder and out of the penis or top of the vagina.
Cervix: A circle like ring of muscle in between the vagina and the womb or uterus. This is at the top of the vagina.
Dysuria: Pain when urinating.
Cervicitis: Inflammation of the cervix; pain on deep sexual penetration, grumbling lower abdominal pain or bleeding after sex.
Pelvic Inflammatory Disease: Infection of the pelvic organs in females including any of: urethra, cervix, uterus, fallopian tubes etc. Long term infection with an STD can cause difficulties with fertility because it scars the reproductive organs internally.
Vesicles: Fluid filled blisters on the surface of the skin. Usually caused by herpes and may be itchy, painful and have a red background.
Common Sexually Transmitted Diseases
What are the common STDs out there?
Chlamydia Trachomatis
We have probably all heard of Chlamydia; it is the most common STD out there.
Chlamydia is an intra-cellular bacteria (it sneakily hides in a cell) that is the commonest cause of STDs. About 5-15% of people have it at any point in time and a great many more have had it before.
Chlamydia does not always cause symptoms: the vast majority of people with it have no idea they have it and will go on to spread it and sometimes many years after they catch it.
Of the people who do have symptoms, chlamydia can cause painful urination or dysuria, discharge, non-specific pain or even pelvic inflammatory disease (PID). PID will be discussed later.
Whatever its form, chlamydia is relatively easy to treat with oral antibiotics (azithromycin 1g in one go or 7 days of doxycycline 100mg tablet twice a day with food). It is important to have another test some time later to ensure that the infection has been cleared.
As will be repeated in this guide, sexual infections can be found in the throat, anus or genitals and so based on your sexual activity, you should test for it in all areas and be treated and then retested in all those areas.
Ureaplasma
‘Ureaplasma parvum and urealyticum’ are bacteria that have been isolated in cultures taken from the genital areas and are thought to sometimes cause STDs of the genitals (urethritis, prostatitis, epididymitis or PID).
There is disagreement in the medical community about when to test and treat for ureaplasma and mycoplasma species however the general idea is to test and treat if a person has symptoms. It is not clear whether routine testing for asymptomatic ureaplasma is necessary.
Mycoplasma
Mycoplasma genitalum and hominis are similar with Ureaplasma as per the above comments. They are both potential causes of genital infections (urethritis, prostatitis, epididymitis or PID) . They will be tested for in comprehensive STD packages or when somebody has symptoms in any body site of concern.
Gonorrhoea
Gonorrhoea or, ‘The Clap’, is an infection similar to Chlamydia but often produces more intense symptoms. Similar to chlamydia, gonorrhoea can remain dormant or asymptomatic in somebody but when it does flare up, it is usually a great deal more dramatic than chlamydia with green or white discharge and pus, fevers, very sore urination.
As my own doctor once said to me ‘You’ll know if you have the clap, you’ll be pissing razor blades’ and I couldn’t put it better myself. Still, like chlamydia, not everybody actually gets symptoms.
Gonorrhoea can be found in the throat, anus or genitals (urethritis, prostatitis, epididymitis or PID) and so based on your sexual activity, you should test for it in all areas and most definitely be treated if found as it is one of the most contagious STDs around.
It is treated with an injection of antibiotics into the muscle of the bottom; called Ceftriaxone or Rocephin. Similar to chlamydia, a repeat test sometime later is essential to ensure the infection has gone.
Can these infections spread further than the genitals to cause more problems?
For some people, the infection will linger at the urethra or testicles but in some, it will spread further up the reproductive structures such as the ovary, fallopian tubes or in males, the prostate.
In men, this can cause infection the testicle (epidydimo-orchitis) or the prostate (prostatitis) causing a red, enlarged and swollen testicle and a deep pain in the abdomen with painful urination. It requires treatment with antibiotics similar to infection or just the urethra but often for a longer period of time.
In women, the reproductive system is more complex and a sexually transmitted infection can infect the cervix, uterus and fallopian tubes. This is called Pelvic Inflammatory Disease.
(Image of female reproductive organs)
What is Pelvic Inflammatory Disease?
Pelvic Inflammatory Disease or PID
is an infection involving the reproductive organs of women caused by STDs such as chlamydia and gonorrhoea.
The uterus, cervix, vagina and fallopian tubes all lie in the lower part of the abdomen near the bowel and so PID, which can infect some or all of these areas, often presents as lower abdominal pain (whether mild, moderate or severe) with or without vaginal discharge, fever and burning urination. It can be very uncomfortable and painful.
Is Pelvic Inflammatory disease a problem?
PID is an important disease as it can cause scarring to the Fallopian tubes in women, even if no symptoms are apparent, and this may cause infertility. After all, a fertilised egg needs to travel from the ovary to the uterus to be fertilised and an infection can cause scarring of these important tubes.
Will I have symptoms if I have PID?
Many times, a woman will not know if she has PID; the infection has taken hold, does not produce symptoms and nobody knows until she has trouble getting pregnant. At this time, a doctor might order an ultrasound of the reproductive organs and find scarring from chronic PID. It is definitely worth getting regular testing to prevent this!
PID can also present with extreme pain and discharge and mimic appendicitis or ectopic pregnancy (where the embryo is not in the uterus but somewhere else and can cause huge pain if it bursts). It is very important for women to have a low threshold for routine STD treatment to ensure this doesn’t occur and is treated should it occur.
When should I start thinking ‘could this be an STD?’
Some women will have pain after sex or a mild abdominal discomfort as the only sign of an STD. This is usually due to cervicitis (infection of the cervix).
Men can have infections, including chlamydia, gonorrhoea and other rarer infections like Donovanosis, in the prostate which can cause less specific symptoms like itchiness of the backside, anal discharge or pain when passing a bowel motion.
More than one infection may be present and it can be associated with other infections such as syphilis or skin ulcers (which will be discussed later).
In a nutshell, even if you do not have any symptoms, go and get tested as you may have still have an STD that you do not know about. Symptoms can be very vague.
Other Common Sexually Transmitted Diseases
What other infections are out there besides chlamydia and gonorrhoea?
Herpes
Herpes is a viral skin infection caused by the Herpes Simplex Virus. It can sometimes cause urethritis or infect other parts of the body like the eye or anus.
Herpes causes small painful and itchy blisters on an area of skin usually on the genitals or lips. The virus infects the nerve supplying a patch of the skin and so a sufferer will get tingling, pain, itchiness going along with the outbreak.
Herpes outbreaks tend to last a few days and then the immune system clears them up. However, the virus remains asleep living in the nerve and will break out again when the immune system is run down.
What kinds of herpes infections are there?
There are two main viruses which can cause herpes outbreaks: HSV1 and HSV2.
In times gone past HSV1 was found on the lips where it commonly causes coldsores whilst HSV2 was found to be on the genitals. Nowadays, HSV1 and 2 are interchangeable probably due to changing oral sex practices.
Herpes; the gift that keeps on giving.
Herpes is never fully cleared from the body. Similar to chicken pox (these viruses are related), it will remain hidden quietly in the nerve roots and reactivate from time to time, spring up and cause painful little red blisters on a patch of skin.
It tends to reactivate over time when somebody is run down or unwell. This is why taking your important B vitamins (especially folate) and looking after your general health will help minimise how often herpes bothers you.
I have herpes, should I panic about it or how to not pass it on?
Herpes is a distressing diagnosis but it need not be.
Over 75% of the population already have HSV either 1 or 2 and the vast majority of cases go undiagnosed.
Of course, herpes is more likely to shed when a person has red sore blisters and has sexual contact with another person. Having said this, even when somebody does not have active herpes sores, the herpes virus can still ‘shed’ from the skin and go to infect a new person.
Viral shedding without symptoms is often the cause of many mysterious new infections. Viral shedding is most likely in the first 12 months after initial infection but far less likely as the years go on and the immune system mounts a response.
What is it like to have herpes?
The first episode of herpes can often be very severe with fever, intense pain, burning urination and feeling unwell. If this occurs, it is best to see your doctor for pain medications, STD screening and antiviral medication which can be taken for 3 days and is effective.
What do I do about recurrent attacks of herpes?
Subsequent attacks are more frequent in the first year but often settle down in following years to become one attack annually or even less as your immune system responds to the virus.
For those with more frequent attacks, antiviral suppression treatment may be helpful; this is a daily tablet regimen to stop herpes outbreaks and stop viral shedding that puts other partners at risk.
What can I do about repeated attacks of herpes?
Many patients worry about passing HSV on, however the vast majority of people will have minimal viral shedding after 12 months. With so many people having some form of HSV in the community, the risk of giving to another person if you do not have blisters is generally quite low.
If you have an outbreak, you should not have sex and seek treatment until it is all cleared. Antiviral herpes medication, taken daily, can also prevent the spread of herpes.
How is herpes spread? Where did I get it?
A common question is whether a herpes infection indicates that a certain partner ‘gave it’ to you.
With the prevalence of HSV so high and the first episode sometimes being quite subtle, it is likely that many people have HSV from a long time back and do not know about it themselves nor have any symptoms.
Reactivation of the virus is common after getting run down or local trauma, such as a ‘night out’ or sexual intercourse itself and so many episodes are not in fact new cases but reactivation.
It is important to mention that 75% of the population have herpes; it is thus 3:1 more likely that the partner you have had intercourse with, or yourself, already had it for some time. Many people simply do not know that they have it. In the context of a new herpes diagnosis, blame is not helpful and it is better to just see your doctor and get treatment.
Whilst herpes can be a devastating diagnosis, it is treatable and rarely serious other than a rash. As the years go on, attacks are less frequent. Early recognition and treatment of primary or reactivated herpes attacks are the mainstay of preventing spread.
More invasive Sexually Transmitted Diseases
So far, we have discussed sexual infections that you catch via skin contact. There are other STDs that can work their way into the body more invasively. They are much rare and not everybody will need to be tested for these. High risk individuals based on sex history will probably be checked for these.
Syphilis
Curiously, for some time, syphilis was the fastest growing disease in Australia.
Syphilis is a very old and well known bacterial disease. It starts with genital contact whereby a ‘chancre’ or special red dot forms on the genitals after you catch it.
The syphilis stays in the body and, if untreated, can spread to other parts of the body over time.
This is known as ‘secondary’ syphilis, latent syphilis and/or ‘tertiary’ syphilis and the dreaded neurosyphilis in the unlucky, untreated few where it goes to the brain to cause psychiatric disease. This is really rare in developed countries.
How can I find out if I have syphilis?
Most syphilis is detected on screening blood tests and it is readily treated with a penicillin G injection into the bottom. It is possible to get syphilis again after one episode (there is no immunity) and can be contracted from oral, anal or vagina sex either receptive or non-receptive.
What do the forms of syphilis look like?
Primary syphilis occurs around 10 days after exposure and involves painless skin lesions; sometimes one, sometimes many and they may be ulcerations or nodule-like lumps. Many times, the first wave of syphilis in a person goes unnoticed and a person presents later on when the syphilis bacteria has gone back into the bloodstream and spread to the rest of the body including the skin to create a whole new set of skin signs.
This is called secondary syphilis.
Secondary syphilis occurs at 6 weeks after exposure and involves a rash on hands and palms, swollen lymph glands and sometimes feeling unwell.
This rash usually clears up in a matter of days, but the person still has syphilis and can pass it on. This is called ‘latent syphilis’ aka where there are no symptoms but syphilis is still present.
The patient is highly infectious until 2 years have passed in the latent stage. By this time, syphilis may be latent for life or 15% go on to have tertiary syphilis which has several possible symptoms; some of which are very severe and permanent neurological problems.
Are syphilis tests always reliable?
Interpreting syphilis blood tests can be tough. The original blood test might have a ‘false positive’ or a ‘false negative’ and the doctor needs to decide if the result is likely true, to then treat and repeat the blood test in 8 weeks to see a trend. Exposed partners should do the same.
What do the various syphilis tests actually mean?
The ‘screening’ tests for syphilis (EIA, TPPA) tend to be positive for life whilst the RPR and VDRL should lower or become negative after successful treatment. If in doubt of what the blood tests mean, repeat the treatment and test again later.
What is the treatment for syphilis?
Treatment involves a shot of Penicillin G. It must be an injection at a high dose, tablets will not work. There are other options for those allergic to penicillin.
I recommend using ice packs on the buttock prior to injection of the medication equally into the left and right buttock. Some patients may have a small ‘reaction’ for a few hours after; this is not an allergy.
Should I have blood tests after treating for syphilis?
Follow up blood tests are essential as reinfection is common and it’s important to know whether treatment is effective lest a new reinfection take place. This is done at 3, 6 and 12 months. If there is sufficient concern for infection based on history, treatment will be given before waiting for the test results and the tests repeated later on to ensure no syphilis has become established.
Hepatitis B and C
Hepatitis B and C are viruses that infect the liver. They get into the body via contact with the blood of another person and so they are the ‘blood borne viruses’. Blood contact is common in sex, even though we cannot always see the blood at the time as it is a tiny amount.
These viruses, alongside HIV, can also be caught from sharing needles or being born with it via transmission from an infected mother during childbirth.
Does Hepatitis B and C go away or stay for life?
Hep B and C both have the ability to infect the liver ‘chronically’ or for life which could result in liver cancer or liver failure in the long term. Thankfully, most people are immune to Hepatitis B due to school vaccinations in most of the western world since the late 90s. Hepatitis C has no vaccination but is more commonly found amongst intravenous drug injectors or those in the commercial sex industry in certain countries.
Can hepatitis B and C be cured?
There are currently treatments available for both hepatitis B and C. Whilst the treatment does not always clear the virus, it makes it inactive and somewhat harmless. In many cases, Hepatitis C can be cured from the right treatment however this is not for all people.
How do I know if I am properly vaccinated against Hepatitis B?
If somebody is unsure of their hepatitis B vaccination status, it is worth doing the blood test to get a definitive answer. Re-vaccination is often required as the vaccine seems to ‘wear off’ in a few people.
Should I be testing for Hepatitis C?
Hepatitis C is not strictly thought of as an STD however it can be passed from blood to blood contact which occurs during sex.
It’s not a routine STD test, but forms part of a comprehensive test or if there is an unknown or higher risk.
Human Immunodeficiency Virus (HIV)
HIV, Human Immunodeficiency Virus, is a virus that attacks the body’s own immune system. This can lead to such low immunity that the body cannot fight infections; this dangerous situation is known as AIDS Acquired Immuno Deficiency Syndrome.
Like hepatitis B and C, HIV is also a blood borne virus and is caught from sex, sharing needles or during childbirth.
For many, HIV is the elephant in the room. Hitting the 1980s like a sledgehammer, HIV was a mysterious, unknown death sentence that swept through communities in the 80s. It is thus no surprise that it is feared by so many people.
HIV is now treatable and causes very little trouble. The presence of HIV in most developed cities is extremely low and whilst there are upwards and downwards trends in HIV, the chance of catching it is still very small for most people.
Who is most likely to catch HIV?
HIV rates are higher in men who have sex with men, IV drug users, those with many sexual partners and those who use sex workers. There are still cases of people contracting HIV from medical settings and many who are born with it; however this is not common in developed countries.
It should be noted that the rate of HIV is higher in the gay community (estimated 6-8%) and can be as high as 40% in the sex worker population in some developing countries.
This risk is often underestimated by patients who seek sexual adventures abroad. The risk of HIV is often underestimated for those engaging in commercial sex workers in certain countries; whilst condoms help protect against HIV, it should be remembered that 1-2% of condoms break and the chance of HIV from such an encounter is higher and frankly, unpredictable.
It is very very unlikely to catch HIV from oral sex, although still technically possible.
As such, people with sexual contact within this population are considered at high risk of HIV transmission and should have regular testing and consider taking tablets to prevent getting HIV; known as PrEP or Pre-Exposure Prophylaxis (see below).
Who should be tested for HIV?
HIV should be tested in any comprehensive STD screen or when the risk cannot be estimated. It takes 8 weeks to come up in a blood test after an exposure and so serial testing may be required. HIV only survives outside the human body for about one second; so it is unlikely to catch it from a dirty syringe on the street or sharing a toothbrush (Hep C can live outside the body for 6 hours though).
Not everybody needs HIV testing. Heterosexual encounters in developed cities with non-high risk individuals is very unlikely to require HIV testing. The focus really is on the high risk groups such as men who have sex with men, intravenous drug users, those engaging in sex workers abroad etc.
Can HIV be treated and is it successful?
HIV can be treated very well using specific ‘antiviral’ tablets that make the HIV level low enough in the blood that you can’t pass it on and lead a normal healthy life.
Once somebody is diagnosed with HIV, they will be started on a combination of medications that are usually so effective that when the blood is tested for HIV, the level is ‘undetectable’ and they actually cannot pass the virus on anymore.
Can you catch HIV from somebody being treated for HIV?
In general, no. Once the HIV level in a positive person is treated and becomes ‘undetectable’, HIV cannot be caught from them.
Should I be afraid of somebody with HIV?
Absolutely not. You cannot contact HIV from touching somebody with HIV. If a person with HIV is taking effective treatment, you cannot catch it from them sexually.
We should not stigmatise those who are HIV positive and if you intend to start a sexual relationship with an HIV positive person, simply see the doctor to arrange a risk assessment. If your partner has undetectable viral load, it is not possible for them to pass it to you.
How can I prevent myself from catching HIV?
Pre-exposure prophylaxis (PrEP) and Post exposure prophylaxis (PEP) are medications that prevent somebody from getting HIV. They work by stopping the HIV from reproducing inside the body.
Pre exposure prophylaxis or PreP is taken before a sexual encounter with an HIV positive contact whilst post exposure prophylaxis or PEP is taken after an exposure to stop the HIV gaining a foothold in the body. Both medications are taken daily.
When might I take PreP or PEP?
Anybody at risk of catching HIV should take PreP. This includes those in the gay community, with a high number of sexual partners or using sex workers. It is taken as a tablet once per day prior to sexual contact to be effective. This tablet is considered to be very very effective.
Human Papillomavirus (HPV) and Genital Warts
What is HPV?
HPV, Human Papillomavirus, is a virus that infects the skin and leads to warts. The virus will enter the skin cells, start reproducing and cause the skin to grow in a disordered lump; this gives the wart its structure.
HPV can cause warts anywhere on the skin and can be caught from touching skin such as in children in the school community. However it can also be caught near or in the genitals due to sexual contact; in this setting, it is called a ‘genital wart’; but it is still the same virus and the same process as any other wart on the body.
If the HPV infection is on the outside of the genitals we can see these warts. However, in women, this virus can also infect the inside of the vagina (including the cervix) where they cannot be seen.
How common is HPV?
Virtually the whole world has been exposed to the HPV family of viruses. Whether it’s shaking hands or getting a common wart as a toddler, genitals warts are simply the same virus family. Genital warts are also really common; some people will carry the virus and seemingly not have warts but they are still able to pass it on to others to give warts.
What is the link between genital warts, or HPV, and cervical cancer?
As discussed before, human papillomavirus can also infect the inside of the vagina and cervix where they cannot be seen.
In some women, the immune system will clear out these viruses and they will disappear. However, certain strains or type of HPV, if not cleared by the immune system, can stay a very long time and cause increasingly disordered skin cell growth. This can result in cervical cancer. There are only a handful of HPV types that are associated with causing cancer; most warts are harmless.
These cancers are slow growing, and take about 10 years to form. This is why women are recommended to have regular checks of the cervix to find the strains of HPV associated with cancer and also to check for any abnormal cells which could lead to cancer if not treated.
These checks are called Papanicolou or Pap smears for short. In Australia, the PAP smear has been replaced with an HPV test of the cervix every 5 years. Only cases positive for ‘high risk’ virus types will go on for further gynaecological tests.
Anal warts and anal cancer from HPV
Just as HPV can infect the inside of the vagina and cervix, they can also infect the outside and inside of the anus. This virus is the cause of anal warts. In the same fashion as cervical cancer, a persistent infection with certain kinds of HPV can lead to anal cancer. This is more common in gay men over the age of 50 who have HIV; these men are recommended to have regular anal checks with a specialist to detect any cancerous HPV or cell changes early and manage them.
Can you be vaccinated to protect against some kinds of HPV that cause cervical cancer?
Gardasil is a vaccination given to children before the age of sexual activity to prevent the kinds of HPV that may cause cervical cancer. This vaccine helps avoid certain kinds of viruses, but only the ones linked to cervical cancer. It does not protect from the more harmless warts in general.
Boys are also encouraged to have the vaccination so that they do not carry the cancer risky HPV types and thus cannot pass them into the population later in life.
It is more useful to give this vaccine prior to the age of sexual activity. This is because HPV is easily spread during sex and it is not known how effective the vaccine is after you already have HPV. Many people choose to take the vaccine at a later age in life anyway.
It should also be noted that even women who have had the Gardasil vaccination should still have regular cervix checks, as no vaccine is 100% effective.
Are genital warts dangerous and how can I treat them?
HPV and their warts are really common. Whilst HPV can lead to cervical cancer in some women and a very specific population of men, they are otherwise quite harmless except for the embarrassment they bring.
Should I get tested for HPV?
It is very important that adult women are screened regularly for cervical cancer and the cancer linked types of HPV. This will involve a test for the presence of the wart causing virus from the cervix.
Outside of this, testing regularly for HPV offers no particular benefit. If you have genital warts, the treatment is focused on treating the actual warts to get rid of them for comfort and to prevent passing it on and otherwise supporting the immune system to clear any HPV.
When should somebody have anal cancer and anal HPV testing?
Men who receive anal sex and are HIV positive are recommended to have anal cancer and HPV testing regularly after the age of 50.
Anal sex is also common amongst heterosexual couples with at least 30% of couples engaging in this form of sex. There is currently no consensus among doctors about screening for anal cancer or HPV in heterosexual circumstances however anybody with concerns or symptoms should speak with their doctor for advice.
Similarly, these guidelines may change over time for men who have sex with men and if there are any concerns or symptoms, a review with a doctor should take place.
How can I get rid of HPV?
Many women will find out from their cervical check that they have HPV. Many men may also obtain testing to see if they have HPV.
Women who have a positive HPV test for the cancer causing types of HPV will need to be closely monitored. It is often helpful to give supplements such as folate and Vitamin B6 to assist the immune system; however they will nonetheless need a repeat check if the cancer-linked HPV virus types are still present and may need further referral to a specialist if they do not go away.
For all other situations, such as the non-cancer causing HPV types, the treatment involves focusing on the immune system and treating any wart that arises. In many cases, there is no need to treat a non-cancer linked HPV type as they are very common and will not lead to disease.
What can I do to get rid of a wart?
The best thing to do is to see your GP to get genital warts and HPV treated; treatment focuses on supporting the immune system to fight the virus or to mechanically get rid of the wart itself.
Many options for getting rid of a wart are available such as cryotherapy (liquid nitrogen sprayed in a gun to freeze the wart to death) and if necessary, numbing the area with cream or a needle and cutting them out. This can be done on the anus area as well although they can be hard to eliminate.
Other things to consider about STDs.
I have a red mark or ‘lesion’ on my genitals; what could it be?
Ulcerating Genital Diseases
The vast majority of ‘spots’ or rashes related to STDs are herpes. Syphilis is another common cause in some groups and the rest of the ulcerative/lesion based STDs are much rarer. Skin conditions occur too.
There are 5 STDs that commonly cause genital lesions:
- Herpes: can be painful, red blisters in crops but it can also be an itchy or even painless lesion
- Syphilis: Can occur as a red ulcer, a papule or multiple of either.
- Donovanosis: This involves one or many red ulcers where the skin breaks down easily.
- Chancroid: very tender little ulcers
- Lymphogranuloma venereum: Red raised ulcer that can get large and also involves the lymph nodes in the groin on one side.
How long does it take for STDs to show up or become positive on tests?
Chlamydia takes about a week to show up after exposure.
Gonorrhoea takes a few days.
Herpes takes about 7-10 days.
Syphilis / HIV / Hepatitis can take longer and so a repeat test at 8 weeks after sexual exposure is recommended.
Therefore, if you do not have symptoms, waiting 7 days after a sexual encounter will make any routine STD screening more valuable.
How are STD tests taken?
Chlamydia and Gonorrhoea can be tested from urine or a small swab of the urethra. Throat or anal sample will require swabs. The nurse helping you with the test will often give you the swabs and you can take them yourself. Any site with discharge should have the sample from the discharge to be more accurate and for females with symptoms a high vaginal swab or cervical swab accurately taken is very helpful for identifying the organism.
For further reading: https://www.cdc.gov/std/tg2015/default.htm
Summary High Risk vs Low Risk
| Population | Recommended Tests | How Often |
|
| • Urine Chlamydia and Gonorrhoea
• +/- Throat swab for gonorrhoea PCR (not culture)
• +/- anal swab chlamydia and gonorrhoea PCR (not culture)
• HIV blood test
• Hep B/C blood test
• Syphilis blood test
• Ulcer based tests if needed | • Before or after a new partner or sexual exposure
• Every 3 months if at high risk
• 1 week after exposure and again at 8 weeks |
|
| • Urine Chlamydia and gonorrhoea
• Mycoplasma/ureaplasma if have symptoms
• +/- HIV/Hep B/C Syphilis if not had for a while or unsure of partner’s history | • Once per year
• 1 week after exposure |
Summary of STDs in a chart
| Disease | Prevalence | Symptoms | Incubation | Test | Who needs? |
| Chlamydia | 5-10% | Burning Discharge >50% no symptoms | 1 week (test 1 week after exposure to be meaningful) | Urine or urethral swab (throat, anus or genitals) | Everybody, new partner or once a year |
| Ureaplasma | uncommon | Usually no symptoms | Not sure | Urethral swab or urine | If symptomatic |
| Mycoplasma hominis | uncommon | Usually no symptoms | Not sure | Urethral swab or urine | If symptomatic |
| Gonorrhoea | <5% | Burning, discharge, sometimes no symptoms | A few days (test 1 week after exposure to be meaningful) | Urine or urethral swab (throat, anus or genitals) | Everybody, new partner or once a year |
| Syphilis | Gay men > Gen pop | Burning, discharge, swollen testicle, sometimes no symptom | Variable, need to repeat test in 8 weeks to see trend | Blood test | Gay men or high risk |
| Hep B | 30% in Asia, otherwise most people are vaccinated | No symptoms in early phase | weeks | Blood test | If unsure of vaccination status or high risk |
| Hep C | Rare | No symptoms in early phase | weeks | Blood test | If unsure of vaccination status or high risk |
| HIV | Very rare | No symptoms | Weeks, need to repeat test at 8 weeks | Blood test | High Risk |
| HPV | 100% | warts | weeks | No test needed | Testing not needed outside of PAP smears |
| Herpes | Common | Blisters, rash | 1 week | No test needed | Testing not recommended (see guide) |
How to Take Swabs and Specimens for STD Checks
Heterosexual Men: Urine or Urethra swabs every 3-12 months
Heterosexual Women: Urine or High Vaginal swabs, must have anus and throat swabs if practices receptive oral sex or receptive anal sex (50% and 30% of women respectively) every 3-12 months
Men who have sex with men: Anal, throat, urine or urethral swabs every 3 months.
| Site | Swab | Medium | Label | Method |
| Vagina* | Swab of the vagina to test for common infections including: Trichomonas, candida, Chlamydia, Gonorrhoea | Swab goes into its own medium in the cap MT4 or UTM (red top with liquid) | Test for: Trichomonas, candida, gonorrhoea, chlamdyia, (Some doctors may also test for ureaplasma and mycoplasma) | *Please see a handout on ‘Self Collected Swab’ to learn more about how to collect your own swabs rather than a doctor or nurse to do it. Steps |
| Throat | Swab of the throat to test for chlamydia, gonorrhoea | MT4 or UTM (red top with liquid) | PCR Chlamydia, gonorrhoea | See Handout Collected by nurse or doctor. Open mouth as wide as possible in good lighting. Tell the patient to say ah. Direct the swab towards the tonsils and avoid any other part of the mouth or tongue. Rub the swab over the tonsils firmly. Gag may happen. Put in MT4 and snap immediately. |
| Anus | Anorectal swab for Gonorrhoea and Chlamydia PCR | MT4 or UTM (red top with liquid) | Test for chlamydia, gonorrhoea by PCR | See Handout Self Collected Swab Open the swab and the culture medium bottle on the toilet deck. Trousers down and one foot up on the closed toilet lid. Hold the swab tightly, insert the soft tip 3-4cm carefully into the anus. Twist the swab slowly for 5-10 seconds and remove. Put in liquid and snap. Do not spill liquid. |
| Urethra* | Swab of the urethra to test for chlamydia and gonorrhoea | MT4 or UTM (red top with liquid) | Test for Gonorrhoea and chlamydia by PCR | See Handout Self Collected Swab Do not urinate for 1 hour before taking the specimen. Open the swab and the culture medium bottle on the toilet deck. Trousers down. Gently squeeze the tip of the penis to see if any discharge. If so, scoop up the discharge with the swab. Hold the swab tightly, insert the soft tip 2-4cm carefully into the urethra (urine hole of penis). Twist the swab slowly for 5-10 seconds and remove. Put in liquid and snap. Do not spill liquid. |
| Urine | Test the first part of the urine flow for gonorrhoea and chlamydia | Yellow urine jar | Test for chlamydia and gonorrhoea by PCR | See Handout Self Collected Specimen Do not clean or wipe genitals. Open jar and fill to 20mL. Close jar and return to nurse. |
Urine is the preferred method of testing for chlamydia and gonorrhoea however Urethra or High vaginal swabs may be done instead of the first pass urine as per your doctor’s instructions.

