
The gut is one of the most important parts of the body. Most people think of our gut as just being a tube where food is absorbed. Actually, our gut has more bacteria than we have cells in our body. Those bacteria are not just enjoying a free ride; they are very active in our health. Not only do they produce many important vitamins, but they regulate much of our nervous and immune systems too. Medical research into the gut is gaining popularity and there is much that is not understood.
Many people suffering from gut problems like loose stools, constipation, bloating, stomach acid and food intolerances will have something wrong with the balance of ‘good’ and ‘bad’ bacterial species in their gut. Technology is now available to measure some of the bacteria in the gut, which helps healthcare practitioners fix a person’s health from the inside out.
Irritable bowel syndrome, heartburn and dysbiosis
Introduction
The gut has 10^14 bacteria. These bacteria give us vitamins, moderate the immune system, produce hormones, help clean out the body, bind toxins, influence digestion and stomach acid and more functions.
When the wrong bacterial balance is present, problems such as bloating, fatigue, autoimmune conditions, hair loss, fatty liver, excess estrogen, malabsorption can result
When there is the wrong bacteria, body wide inflammation and autoimmune conditions can also result.
Fasting, eating a healthy diet with vegetables and minimising processed foods help keep the gut happy.

What is dysbiosis?
The human gut contains 10^14 bacteria, over 1000 different species, that interact with our body to influence our health. These bacteria play an important role in helping us to:
- Absorb vitamins,
- Regulate inflammation in the body,
- Manage gas levels and stool habits
- Influence stomach acid
- Enhance food digestion
- Interact with hormones
- Prevent gastroenteritis or gut infections
- Related to multiple disease states (allergy, Crohn’s disease)
- Moderates the immune system
The microbiome is influenced by many factors including our general health, habits, what we eat and when we eat as well as environmental and genetic factors.
Dysbiosis refers to a relative imbalance in these bacterial populations that affects our health in a negative way. There are many kinds of dysbioses that produce a range of symptoms and they require unique, tailored treatment. In this pamphlet, we discuss gut dysbiosis however vaginal, oral (or dental) and skin dysbioses also occur.
What is Small Intestinal Bacterial Overgrowth
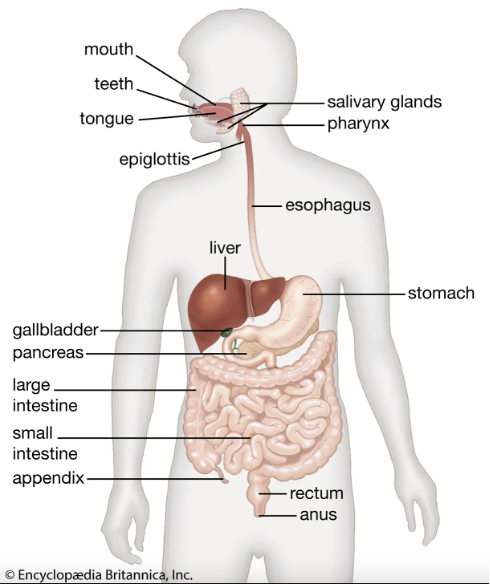
The small intestine comes before the large intestine and is the major site for vitamin and nutrient absorption. The large intestine is also known as the colon. Much of dysbiosis describes the relative populations of bacteria that are in the colon or the large intestine which is further down and has a different function to the small intestine. The large intestine has higher amounts of bacteria than the small intestine.
Dysbiosis higher up in the gut (towards the mouth) in the small intestine can produce a clinical syndrome called Small Intestine Bacterial Overgrowth or SIBO. As the name suggests, a relative imbalance in bacterial types can then influence gas, stomach acid, vitamin absorption and body health in a unique way.
People with Irritable Bowel Syndrome, a syndrome describing gut problems including bloating, nausea, constipation, vomiting, fatigue, flatus, belching, have 5 times the likelihood of having SIBO. SIBO actually presents with similar symptoms and your practitioner will make an evaluation on whether you should be tested for SIBO or whole gut dysbiosis.
SIBO is a type of dysbiosis and requires a unique treatment that considers related problems such as a lack of stomach acid, breakdown in gut defences, poor pancreatic digestive enzyme function and gut motility which means how fast the gut contracts to push things along. Treatment is complex and is an investment; it takes time to use supplements and dietary change to re-balance the gut.
Testing for SIBO
If you have bloating, belching, flatus, constipation, diarrhoea, indigestion, stomach acid etc. your practitioner may consider SIBO as a diagnosis.
SIBO is diagnosed by a breath test looking for high levels of hydrogen after ingesting lactulose. The test can also be helpful in finding methane gas which can be related to a dysbiosis that causes constipation. The test involves drinking lactulose, a sugar, and then recording the presence of hydrogen and methane from your breath. If you have SIBO, bacteria will create hydrogen and this will be captured in the breath test.
SIBO breath testing takes time. This is because the lactulose moves through the gut over a few hours; the jejunum starts earlier and by 100 minutes the test will indicate the ileum, where SIBO often takes place.
Completing the test properly is essential for a good diagnosis; a video tutorial is available from the pathology company and patients are strongly advised to watch it prior to completing the test.
SIBO is associated with many other gut conditions and each case is different and unique to the patient’s gut microbiome and body. It is generally superior to do both SIBO breath testing and a GI Map, which is a stool test that uses DNA PCR technology to check what kinds of bacteria are in your gut, to help assess the whole case and direct treatment.
What are the symptoms of dysbiosis?
The interaction of our gut biome and the body’s functions are broad and diverse. Many of the symptoms of dysbiosis are common to many other medical problems and so seeking professional assistance is vital.
Dysbiosis can present with gut symptoms such as:
- Bloating
- Indigestion
- Heartburn
- Constipation or loose stools
- Typical symptoms of irritable bowel syndrome
- Metabolic syndrome
- Fatigue
- Mental health or cognitive symptoms (brain fog)
- Hair loss
- Acne
Problems outside the gut such as acne, fatigue, hair loss, weight gain to name a few may also be influenced by the gut biome. Once again, SIBO is a special kind of dysbiosis.
What leads to dysbiosis?
Gut bacteria thrive by eating fibre and indigestible plant material. They use this to create molecules for their own survival. Furthermore, anything ingested that harms bacteria such as chlorine in the water, antibiotics, chemicals in hygiene products or artificial food chemicals like sweetener can alter the biome composition. This is because naturally occurring bacteria are not used to these chemicals.
The western diet is often low in fibre diversity, low in polyphenols, has many food additives, high exposure to environmental chemicals, low in microbiota accessible carbohydrates and departs significantly from what our bodies are used to eating.
Many people develop gut problems after antibiotic ingestion or a gut infection. Once again, these alter the gut bacterial populations and predispose to dysbiosis.
How can dysbiosis be treated?
Dysbiosis treatment is unique to every person and their circumstances; having an informative diagnosis and choosing appropriate treatments in sequence is essential for a good outcome.
Treatment generally follows several phases to optimise liver and body, remove the dysbiosis using antimicrobials, re-populate the gut with good bacteria using probiotics and prebiotics, repair the gut using supplements and finally to maintain with good diet and probiotic use.
During the treatment, assisting any digestive problems is important as the gut employs digestive chemicals like acid or pancreas enzymes, to maintain itself. Good digestion is indistinguishable from a healthy gut and so would be addressed as a part of any gut concern.
Dysbiosis Treatment Regimens
This is just an example and treatment is based on body status, vitamin deficiencies and SIBO treatment differs to other dysbiosis treatments.
Treatments are often staggered in phases with one phase beginning two-four weeks before the next phase but overlapping. Your doctor will advise on the treatment duration for each step.

Timeline of Treatment Phases
First phase: (Start Week 1) Optimise health and body function
Second phase: (Start week 3) remove the dysbiosis and kill the bad bacteria
Third phase: (Start week 5) recolonize the gut with good bacteria
Fourth phase: (Start week 7) heal the gut
Fifth phase: (Start week 9) prevent recurrence
#The phases do not only last for 2 weeks; they begin 2 weeks apart and are run together.
First phase: (Start Week 1)
Optimise health and body function
Lifestyle, nutrition, sleep, exercise and stress.
Restore any vitamin or hormone deficiencies or imbalance.
Firstly, treat any parasites and get this out of the way as they will make other treatments much harder.
Prepare the liver and other systems for detox [E.g supplements such as berberine, NAC, dandelion root and cut alcohol]
Use digestive enzymes such as bitters, apple cider vinegar, pancreatic enzymes, Betaine (a kind of stomach acid), zinc carnosine etc. to address any maldigestion and assist gut function.
Remove any foods from diet that cause inflammation; usually gluten and dairy are minimised and follow low FODMAP diet.
No snacking between meals is allowed during dysbiosis treatment. The gut must be allowed to empty as best as possible.
14 days before starting next phase; continue into next phase 6 weeks minimum or until bottle runs out
Second phase: (Start week 3)
Remove the dysbiosis and kill the bad bacteria
Antibiotics that are gut limited, such as rifaximin, are used for 14 days.
Herbal antimicrobials against bacteria are commonly used in conjunction with rifaximin such as: caprylic acid, garlic oil, oil of Oregano, olive seed extract, grape seed extract, berberine.
Herbal antimicrobials need to be used for longer and use multiple ones.
Herbal Antifungals may be used if needed such as: caprylic acid, oil of oregano, Nigella sativa (black cumin) seed oil, olive oil extract, grapefruit seed extract.
Herbal Antiparasitics may also be used: wormwood, olive leaf extract, grapefruit seed extract, and berberine.
This phase is started for two weeks before moving on to the next phase however will continue until at least 6 weeks for the herbal products or further, until the bottle runs out. Each case is different and your doctor will advise you.
Third phase: (Start week 5)
Recolonize the gut with good bacteria
This phase involves using probiotics and prebiotics to enhance good bacteria in the gut.
This phase is started after the use of rifaximin, or 14 days after starting antimicrobial herbal treatments and then run concurrently until the previous phase runs out (usually 6 weeks or when the bottle finishes)
Probiotics: Can use Saccharomyces Boulardii yeast at 5 million CFU three times per day after meals OR an appropriate higher dose broad probiotic.
Probiotics are best taken 2 hours before or after meals to help the good bacteria make it past the digestive system to the colon.
Prebiotics: Modified Citrus Pectin, Polybiotic powder, Lactulose
This phase is run for 14 days before starting the next phase; however the recolonisation phase should be continued for about 3 months concurrently with the next phase
Fourth phase: (Start week 7)
Heal the gut
This phase takes place after the initiation of prebiotics and probiotics. It involves using gut friendly substances to heal the gut. This may simply be an extension of the prebiotics used in phase 3 or more advanced measures such as L-glutamine or aloe vera to heal the gut.
For those with SIBO, the use of a methane moderating treatment or mood enhancing adjunct is employed here.
Fifth phase: (Start week 9)
Prevent recurrence
The fifth phase describes a general set of habits that help prevent dysbiosis returning.
Maintain a clean diet, and healthy body.
Maintenance probiotic for a while:
For methane SIBO cases, long-term methane treatments may be helpful.
Many practitioners treat dysbiosis in different ways however the principles are broadly the same. It is always recommended to seek professional help from your practitioner.
Tips on taking the supplements?
Digestive enzymes are best taken 10 minutes before you eat on an empty stomach.
Antimicrobials are best to be taken with meals as directed above and for 14 days. It is better not to use probiotics in this first 14 days.
After 14 days of this treatment phase, probiotic and prebiotics are generally taken on an empty stomach (2 hours before or after eating) for one month at least up to 2 months based on the need.
It is important not to snack so that your gut can rest and clean itself up
Following this, maintenance therapy is continued as needed; probiotics taken on empty stomach for best effect.
During therapy, you will be more sensitive to gluten and it is recommended to be gluten free as possible.
Some people experience marked fatigue during the kill phase in phase 2. This is because the antimicrobials are killing bad bacteria that have lived in the gut for a while.
It may be helpful to take a ‘binder’, a supplement that helps bind the toxic debris of dead bacteria so that your immune system does not react and make you tired.
Constipation therapy may be necessary for some people using Magnesium oxide or lactulose.
Index of Treatments and What they Do:
Body Support Treatments
Digestive Enzymes are supplements which help with digestion. They may include stomach acid (HCL), Zinc or pancreatic enzymes. Breaking down the food is important as it prevents some of the fermentation that may occur from less digested food particles and a proper pH in the gut is essential for vitamin absorption.
Zinc Carnosine is a combined zinc product. Zinc is commonly deficient in the developed world and is an important mineral for many enzyme reactions around the body. Chiefly, zinc is required for good stomach acid and carnosine is helpful for gut health. Zinc carnosine is the preferred compound for patients with digestion issues, SIBO, dysbiosis or gut issues.
Berberine is a herbal treatment that is very helpful for the gut and to reduce toxicity. It not only promotes the good bacteria, but blocks the toxins from the gut going to the liver to cause fatty liver, high cholesterol, high sugar and high blood pressure. It is a key treatment.
NAC is used to ‘detox’ the liver. Because we are killing bad bacteria there will be toxins hitting the liver and NAC will assist the liver cope with this.
Phosphatidyl Choline is a choline supplement; During the phase in which somebody is being treated for high homocysteine and a gut condition, this is helpful.
Disclaimer
This article is a reflection on an approach to dysbiosis as a wider topic. Brand names of supplements are used to give an example of a treatment approach and is not meant to constitute medical advice or treatment advice. Other brands and treatments abound and readers should speak to their healthcare practitioner regarding their own circumstances.
Reference
Belizário JE, Faintuch J. Microbiome and Gut Dysbiosis. Exp Suppl. 2018;109:459- 476. doi:10.1007/978-3-319-74932-7_13
Bull MJ, Plummer NT. Part 2: Treatments for Chronic Gastrointestinal Disease and Gut Dysbiosis. Integr Med (Encinitas). 2015;14(1):25-33.
DeGruttola AK, Low D, Mizoguchi A, Mizoguchi E. Current Understanding of Dysbiosis in Disease in Human and Animal Models. Inflamm Bowel Dis. 2016;22(5):1137-1150. doi:10.1097/MIB.0000000000000750
Gagliardi A, Totino V, Cacciotti F, et al. Rebuilding the Gut Microbiota Ecosystem. Int J Environ Res Public Health. 2018;15(8):1679. Published 2018 Aug 7. doi:10.3390/ijerph15081679
Wilkins LJ, Monga M, Miller AW. Defining Dysbiosis for a Cluster of Chronic Diseases.
Sci Rep. 2019;9(1):12918. Published 2019 Sep 9. doi:10.1038/s41598-019-49452-y

